You are here:
- Procedures / Corneal transplantatino for Fuchs' dystrophy
Corneal Transplantation for Fuchs' Dystrophy
What is Fuchs’ Dystrophy?
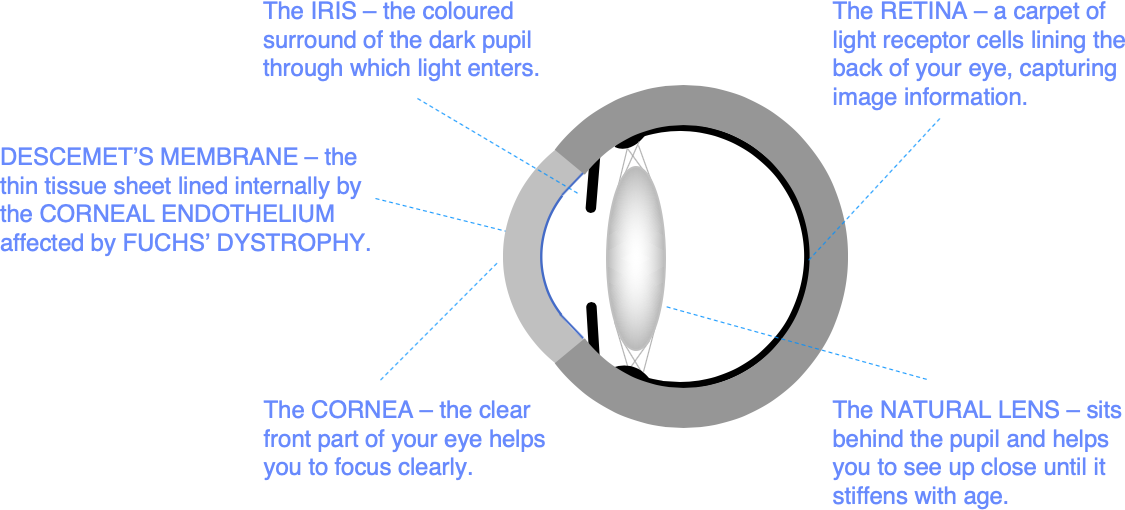
The cornea is maintained in a state of relative dehydration by an important layer of pump cells lining the back surface called the corneal endothelium. If this cell layer fails, the cornea absorbs water from inside the eye like a sponge, becoming waterlogged and misty. The medical term for this waterlogging is corneal oedema.
If you are starting to develop corneal endothelial failure, you might notice morning misting – misty vision first thing in the morning. This misty vision takes longer to clear with time, as corneal endothelial pump function deteriorates. Without treatment, you will eventually find that the vision is blurry all day. You may also have intermittent stinging pain caused by tiny blisters forming on the eye surface.
Fuchs’ Corneal Endothelial Dystrophy is a relatively common inherited condition in which corneal endothelial function declines at a faster than normal rate. If you have Fuchs’ dystrophy, you may start to experience morning misting, and you may need a corneal transplant to restore a healthy corneal endothelium and clear vision. The age at which morning misting becomes a problem varies greatly, and many patients with Fuchs’ Dystrophy are either never affected, or only affected late in life.
You may also have problems with glare and light scatter. This is because Fuchs’ dystrophy also affects a very thin layer called Descemet’s membrane which supports the endothelial cell layer. You can think of Descemet’s membrane as the underlay for the carpet of endothelial cells lining the back of the cornea. Descemet’s membrane is normally smooth and clear. But it becomes more like a cobbled street in Fuchs’ dystrophy, as the abnormal endothelial cells leave behind bumpy deposits called guttata that scatter light. A few guttata are no problem, but dense guttata in later stage Fuchs’ dystrophy can cause disabling glare.
Corneal guttata are often noticed in a routine eye examination – up to 4% of people have at least some signs of Fuchs’ dystrophy, but many patients are only very mildly affected, and never require any treatment.
You don’t have to have Fuchs’ Dystrophy to have corneal endothelial failure. Other common causes of endothelial cell loss are eye injury and any form of surgery on the inside of the eye. After cataract surgery for example, we typically lose at least 5% of our corneal endothelial cells. This is usually no problem; but if you have Fuchs’ dystrophy and you are already running out of endothelial cells, cataract surgery may result in the need for a corneal transplant.
What is DMEK?
In modern corneal transplantation for Fuchs’ Dystrophy and other causes of corneal endothelial failure, rather than replacing the whole of the cornea, we simply replace the back layers that are unhealthy. These are the endothelial cell layer, and Descemet’s membrane.
Descemet’s membrane can be peeled away from the back of the cornea relatively easily, it will also stick back on with no glue or stitches if it is compressed back into place with an air bubble – a bit like sticking a stamp to an envelope. This means we can treat corneal endothelial failure with a relatively simple operation in which the unhealthy Descemet’s membrane and endothelial cells are peeled away, and replaced by healthy donor tissue. This operation is called Descemet’s membrane endothelial keratoplasty or DMEK.
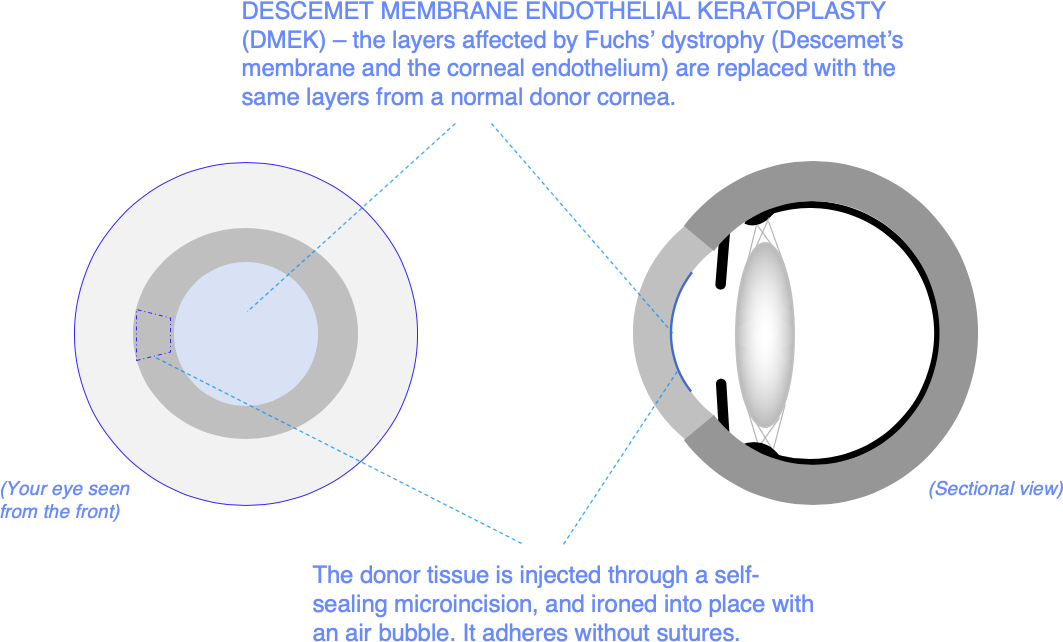
DMEK takes about 30-45 minutes and is normally done under local anaesthetic. The operation is keyhole surgery, using small, self-sealing entries into the eye that are the same as those used in modern cataract surgery. This means that you can quickly get back to normal activity after the operation.
We often combine DMEK with other operations including cataract surgery. We will advise you of the need for any further procedures at your initial consultation.
What are the benefits of DMEK?
Common problems for patients with Fuchs’ dystrophy are increasing visual blur, morning misting, glare and light scatter. DMEK is normally very successful at restoring clear, good quality vision.
Your eye comfort may also be improved. When corneal waterlogging is at an advanced stage, painful blisters can form on the eye surface. DMEK normalises corneal hydration, and these blisters resolve.
We normally recommend surgery before you reach the stage at which eye comfort is a problem.
Who is suitable for DMEK?
If you have been told you have Fuchs’ dystrophy at a routine eye examination, but you are not having any problems with your vision or your eye comfort, you do not need any active treatment. You should simply continue with annual eye health checks under the care of your local optician.
If you are having problems with light scatter, or you are starting to experience morning misting. You may need DMEK.
If you have corneal endothelial failure for reasons other than Fuchs’ dystrophy, including failure of a previous corneal transplant, DMEK is often the best treatment option.
The tests we do at your initial consultation will help us to give you clear advice about your suitability for treatment.
What if I have cataracts too?
People with Fuchs’ Dystrophy often develop cataracts (age related loss of clarity of the natural lens) earlier in life than average. In the jargon, there is some ‘genetic linkage’ between early cataract development and Fuchs’ dystrophy.
If you have been told you have Fuchs’ dystrophy and are having problems with misty vision or light scatter, you may simply need cataract surgery. But if morning misting is already a problem, or if microscopic blisters are present on the eye surface (a sign of corneal waterlogging), DMEK can be combined with cataract surgery to avoid a delayed visual recovery.
We normally do a 3D scan of your cornea called corneal tomography at your initial consultation. If that scan shows thickening of the centre of your cornea due to corneal waterlogging, this is another reliable indication that you will need DMEK combined with cataract surgery in order to restore clear vision.
What are the alternatives?
PK
If you have problems with the other layers of the cornea as well as endothelial failure, your best option may be a conventional full thickness corneal transplant, also called penetrating keratoplasty or PK.
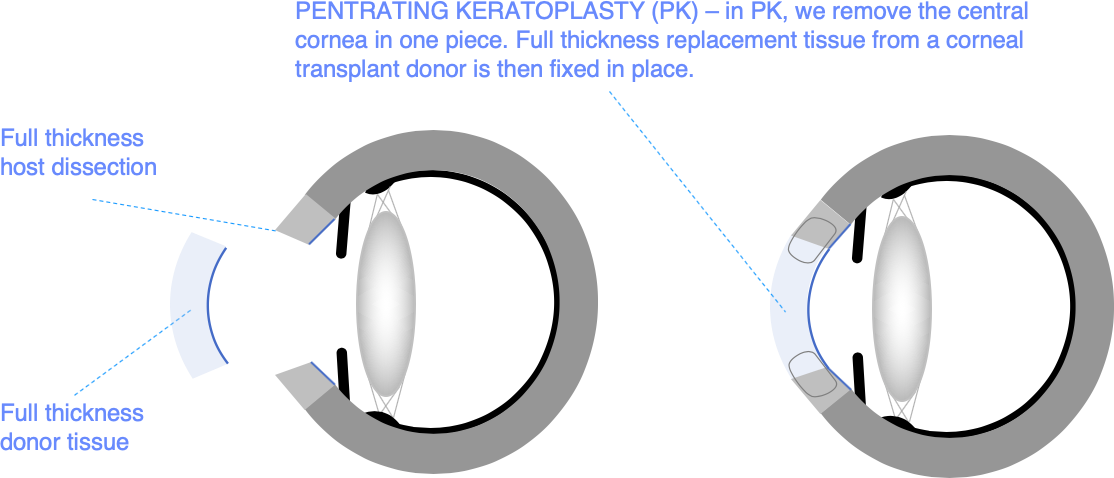
In conventional corneal transplantation, the full thickness of the front of the eye wall is replaced by a disc shaped piece of donor corneal tissue which is sewn into place. The circular wound heals gradually, and the sutures are normally removed one to two years after surgery.
DSAEK
DSAEK is the same as DMEK, but the replacement tissue includes a thin layer of the leathery tissue (stroma) that gives the eye wall its strength.
Including this additional supporting layer makes the operation easier technically, and for this reason, it is still an option that many corneal surgeons prefer. But the extra donor tissue increases the risk of corneal transplant rejection. This is why we now normally recommend DMEK.
DSO
Fuchs’ dystrophy is very variable. For some patients, only the central Descemet’s membrane appears to be involved, and the endothelial layer can be relatively normal outside this central zone. If you are in this group with the so-called ‘central phenotype’, you may be suitable for an operation called Descemet’s Stripping Only or DSO. This operation is identical to the first part of DMEK, but only the abnormal central 4-5mm of Descemet’s membrane is removed, and no donor tissue is implanted. Instead, we rely on your own endothelial cells to migrate over the centre of the cornea to restore an intact pump layer.
DSO is easy to do, and works in about 80% of people with the ‘central phenotype’ of Fuchs’ dystrophy. But the recovery is slower than DMEK, and you may need a DMEK if the cornea is not clear by 3 months after DSO.
A new eye drop called Ripasudil has been used to improve results in DSO by stimulating endothelial cell migration. Early evidence suggests that Ripasudil may be helpful, but we do not yet know whether it helps everyone who has DSO. Ripasudil is a licensed glaucoma eye drop in Japan, but is not yet routinely available in the UK.
If you are suitable for DSO, we will discuss the pros and cons of this treatment option versus DMEK at your initial consultation.
No treatment
Corneal endothelial failure gets steadily worse without treatment, and some of the changes in the cornea associated with long-term waterlogging cannot be reversed. We therefore normally recommend that DMEK or an alternative treatment is performed before morning misting turns into permanent blur, and certainly before painful eye surface blisters start to form.
How is DMEK performed?
We normally perform DMEK using drop anaesthetic supplemented by an injection in the back of your hand to relax you if required. Anaesthetic may also be washed around the back of the eye to prevent excessive eye movement. A spring clip holding the eyelids apart allows you to blink safely during surgery.
We will be looking through a microscope to perform the surgery. You will be lying down under a surgical tent with fresh air coming in underneath. A sticky plastic drape covers the skin around your eye and sticks the eyelashes out of the way.
If we are combining DMEK with cataract surgery or if you have no other problems with the eye other than Fuchs’ dystrophy, strong pupil dilating drugs are given as drops or as a pellet placed under the lower eyelid to prepare your eye for surgery.
Essential steps in DMEK surgery are:
-
Entry points – formation of small, self-sealing entry points in the front of your eye at the junction of the white of the eye and the cornea
-
Descemetorhexis – removal of a circular disc of unhealthy Descemet’s membrane from the centre of the back of your cornea
-
Donor injection – healthy Descemet’s membrane from a donor cornea is dyed blue and rolls up spontaneously when it is immersed in liquid. We inject this rolled-up donor tissue into the front chamber of your eye through one of the small, self-sealing entry points.
-
Donor unrolling – we unroll the new Descemet’s membrane in your eye using injected jets of fluid and fluid waves created by tapping gently on your eye surface, making sure that the side with the endothelial (pump) cell lining is facing away from the back of the cornea.
-
Donor centration – we inject a small air bubble underneath the correctly orientated donor tissue to float it into light contact with the back of your cornea. We fine tune its position to make sure that it is well centred. You may be aware of more gentle tapping on the front of your eye at this point.
-
Air compression – when the donor tissue position is optimal, we stick it into place by completely filling the front of your eye with air.
-
Air exchange – we remove most of the air and replace it with fluid to ensure that the air bubble will not block fluid flow around your eye after the surgery causing a painful rise in eye fluid pressure.
We normally give you instructions about posturing so as to support the DMEK corneal graft in place at the end of the operation.
What are the risks?
In all forms of eye surgery, problems can occur during the operation or afterwards in the healing period. Problems can result in permanent, serious loss of vision (vision worse than the driving standard in the affected eye that cannot be corrected with glasses or contact lenses). More commonly, problems can be corrected with changes in medication or additional surgery. Typically, these additional operations feel like the original surgery and have a similar recovery period.
Loss of vision
DMEK is performed to prevent permanent, serious loss of vision, but permanent visual loss can still occur due to complications resulting from surgery that damage the retina or the optic nerve. This may mean vision worse than the driving standard or, in some cases, complete loss of vision in the affected eye.
Many patients undergoing DMEK have pre-existing problems with the retina or optic nerve such as macular degeneration or glaucoma that can affect the visual recovery from surgery. If the cornea is cloudy because of waterlogging, it is sometimes not possible to fully assess the health of your eye before your surgery.
If you have no problems with the eye other than Fuchs’ dystrophy or cataract, the risk of permanent serious visual loss is low.
Additional surgery
Your DMEK graft has to be fully attached for the new endothelial cells to pump effectively and clear your vision. We often find partial detachment of the DMEK graft at your first postoperative visit.
If your DMEK graft is mostly attached (>70%) at the first visit, we can be confident that full attachment will occur spontaneously, although this may take 2-3 weeks. If you have a larger detachment, or spontaneous re-attachment is not occurring fast enough, we often inject more air and ask you to do some more posturing to position the air bubble under the graft effectively. Repeat air injection or ‘re-bubbling’ is low risk, not painful, and is normally done during the clinic consultation. We need to re-bubble about 1 in 6 cases. Re-bubbling can be repeated if necessary, and there is no difference in final results between cases requiring re-bubbling and those that do not.
Graft failure
In about 1 in 20 cases, the cornea fails to clear after DMEK surgery. This is called primary graft failure. If vision is not improving by one month after your DMEK operation, this may be the reason.
DMEK is a relatively new operation, and we do not yet know how long we can expect DMEK grafts to last after successful surgery. Graft survival should be at least as good as for PK (conventional corneal transplantation) however, because we know that the rates of two common problems that can lead to graft failure, graft rejection and steroid induced glaucoma, are both lower in DMEK. Approximately 75% of corneas treated with PK for Fuchs’ dystrophy stay clear for at least 5 years after surgery.
If your vision fails to clear or becomes blurry again years later because of graft failure, repeat DMEK surgery is normally possible.
Graft rejection
Transplant rejection is an inflammatory reaction to donor cells caused by your body’s immune system.
Unlike, say, kidney or heart transplantation, most patients treated with corneal transplants do not benefit from either tissue matching (tissue from a donor with some cell markers similar to your own) or systemic immunosuppression (powerful drugs to suppress your immune system).
Possibly because only one cell type (corneal endothelial cells) is transplanted in DMEK, rejection rates are significantly lower than for the other types of corneal transplant (PK and DSAEK) that are used to treat Fuchs’ Dystrophy.
About 1 patient in 50 has a corneal transplant rejection episode after DMEK. To reduce this risk, you should ensure that you take your postoperative drops as instructed after surgery. We normally continue steroid eye drops in a low dose for two years after surgery.
If you experience Redness, Sensitivity to light, Visual blurring, or Pain (“RSVP”) at any stage after corneal transplantation, you should reattend via the Casualty Service without delay to make sure that you do not have a graft rejection episode. Graft rejection can normally be treated successfully with an increase in steroid drop treatment, but delays in treatment or repeated episodes can lead to graft failure.
There are reports that the influenza vaccination (‘flu vaccine’) may precipitate a corneal graft rejection episode. The risk of this occurring is likely to be low, and you should certainly not refuse vaccination because you are worried about this. To cover this risk, we currently advise that you should ask your local doctor to prescribe a 2-week course of steroid eye drops (Dexamethasone 0.1% or Pred Forte) to be taken 4 times daily from the day of vaccination.
Steroid induced glaucoma
Steroid eye drops help protect from rejection, but they can cause the fluid pressure in your eye to rise. We screen for this with an eye pressure test at your postoperative clinic visits, and we often prescribe additional eye drops to lower the fluid pressure if we find that it is high. If left untreated, high fluid pressure can damage the optic nerve at the back of your eye. So, it is important to attend your hospital review visits, and to take any additional eye drops that we prescribe in the period in which we need to continue with steroid eye drops.
What are the side effects?
Side effects are problems which most patients experience to some degree after surgery. They normally improve with time, but do not always resolve completely.
Vision
Temporary blurring of vision is normal after DMEK, but most patients find that the vision clears in the first month after surgery. Your vision may initially be worse after surgery than before, and the speed of recovery is very variable. If you have blurred vision at first, it does not mean that you are not going to get a good final visual result.
Eye comfort
Some eye surface discomfort is common in the early months after most forms of eye surgery. This is usually mild after DMEK, and highly variable – often affecting one eye more than the other. Treatment and prevention are based on making sure your eye surface is healthy before and after surgery. Lubricant eye drops can be helpful, and can be taken safely in addition to your other medication when required. For patients with a normal eye surface prior to surgery, lasting problems are unusual.
Eye Appearance
Red blotches are often visible on the white of the eye after any form of eye surgery. These are called subconjunctival haemorrhages, and are caused by a small leak of blood under the mucous membrane covering the white part of eye wall. Although they can be quite unsightly, red blotches are temporary, and do not affect eye health; but they can take up to 6 weeks to go away completely.
Will DMEK affect my future eye care?
If you develop a new eye health problem in later life, DMEK should not prevent you having successful treatment. Common eye health problems like cataract, glaucoma, diabetic retinopathy, and age-related macular degeneration can be monitored and treated as normal after DMEK.
Future surgical treatment can sometimes precipitate graft failure. If surgery is planned, we can give you advice on the risk of graft failure by checking the health of your corneal endothelial cell layer with specialised imaging tests.
We normally recommend that you continue to review your eye health once a year under the care of your local optometrist after you have been discharged from routine postoperative clinic review at Moorfields.
How can I reduce the risk of problems?
Most patients have DMEK under local anaesthetic. You can eat and drink normally before surgery, and should take any regular medication as usual.
We work with an anaesthetist to monitor your health during surgery and optimize your comfort, administering sedation where necessary. Keep your breathing calm, stay as relaxed as you can, and try to keep your head still after we have positioned it comfortably.
You can help us apply the drape and stick your eyelashes out of the way by opening both your eyes wide at the beginning of surgery. You should clean off any make-up or moisturising cream before surgery to help the adhesive drape to stick properly. Blinking is no problem after draping is complete. Just look straight up ahead to the bright operating light with both eyes open, but blink when you need to. Looking up to the bright microscope light helps to keep your eyes in the best position.
We will talk you through the procedure, encouraging you at every stage. Let us know if you feel any discomfort, and tell us if you need to cough, sneeze or take a break.
A clear plastic shield is normally taped over the eye at the end of surgery to protect the eye on the way home. Nursing staff will show you how to wear the eye shield at night (normally for 1 week after DMEK).
Avoid rubbing your eye in the first week after treatment. Eye rubbing in the early days after surgery may cause your DMEK graft to detach. If we have left an air bubble in your eye to help iron the DMEK graft out against the back of the cornea, we will give you instructions about posturing in the 2 days after surgery (or after re-bubbling). This normally involves lying on your back looking up to the ceiling to help locate the bubble beneath your DMEK graft, floating it up against the back of the cornea. You can take breaks when needed, and you do not need to posture when you are travelling home. If possible, you should sleep on your back for the first 2 nights after surgery.
You can wash and shower normally from day one after surgery. We recommend no swimming for a week and no contact sports for a month. Non-contact sports such as gym and jogging can be resumed once you have finished your period of posturing after surgery. It is safe to start driving again when you can read a number plate at 20 yards with both eyes open and you are reasonably comfortable with your new vision.
Set a smart phone reminder and use the antibiotic and anti-inflammatory drops as prescribed to help the eyes to heal well. It is good to leave at least 2 minutes between different types of eye drop so that they each absorb well before the next drop is applied. If you miss the first time or you are not sure, applying a second eye drop is no problem.
Mild discomfort is normal in the first few days after surgery. But you should contact us without delay if you have building, aching pain in the eye (like a headache in the eye). This could mean that an air bubble left in your eye is blocking fluid flow through your pupil. Try sitting up to move the bubble if you have been lying down, but if the pain does not resolve promptly, you should let us know – even if it is the middle of the night. This problem called ‘pupil block glaucoma’ is uncommon, particularly with the DMEK techniques we now use, but it can still occur.
The Eye Casualty Department at Moorfields Eye Hospital is open for emergency review 24 hours a day, 7 days a week.
Remember ‘RSVP’ – increasing redness, sensitivity to light, visual blurring, or pain. These are the warning signs of a corneal transplant rejection episode. If you experience any of these symptoms, it is best to attend via the Casualty Service to make sure you do not need additional treatment.
You may not be aware of a problem that requires treatment in the healing phase. So, make sure you attend your review appointments even if your eyes feel good.
Appointments and enquiries
To arrange a private consultation, please telephone Angelique Thomas on 020 7566 2156 or 07484 081815 (or from outside the UK +44 20 7566 2156 or +44 7484 081815) or email moorfields.ballan@nhs.net
For NHS treatment with Mr Allan’s team at Moorfields, you will need a referral from your GP or Ophthalmic Surgeon. Referrals should be addressed to Mr Bruce Allan, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital, City Rd, London EC1V 2PD. If you have any difficulty with your NHS referral, please call Barbara Stacey, NHS secretary to Mr Allan on 020 7566 2320, or email barbarastacey@nhs.net.
