You are here:
- Procedures / Endothelial keratoplasty
Endothelial keratoplasty: corneal transplantation for Fuchs dystrophy
DMEK for Fuchs Dystrophy
Fuch's dystrophy and corneal endothelial failure
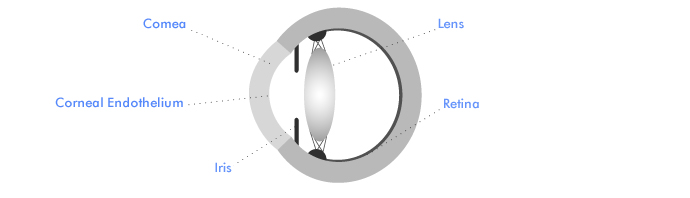
The cornea is maintained in a state of relative dehydration by an important layer of pump cells lining the back of the cornea called the corneal endothelium. We are born with an ample supply of these cells, but endothelial cell density decreases slowly with age. If cell density drops below a safe minimum level, the pump action of the endothelial cell layer becomes insufficient, and the cornea starts to become waterlogged and misty. The medical term for this waterlogging is corneal oedema. In the early stages of corneal endothelial failure, patients typically experience morning misting - cloudy vision which tends to clear later in the day.
Fuch's Corneal Endothelial Dystrophy is a relatively common inherited condition in which endothelial function declines at a faster than normal rate. Most of us are unlikely to live long enough to experience any problems with corneal endothelial failure; but some patients with Fuch's Dystrophy require a corneal transplant to restore a healthy corneal endothelium and clear vision. The age at which morning misting becomes a problem varies greatly, and many patients with Fuch's Dystrophy are either never affected, or only affected late in life.
Other common causes of endothelial cell loss are eye injury and any form of surgery on the inside of the eye. After cataract surgery for example, we typically lose at least 5% of our corneal endothelial cells. This is usually no problem; but if cataract surgery is carried out in patients with a diminished reserve of corneal endothelial function, the cornea may become misty as a result. Eye surgeons will often warn patients with Fuch's Dystrophy that cataract surgery may result in the need for a corneal transplant. If morning misting is already a problem, or if microscopic blisters are present on the eye surface (a sign of corneal waterlogging) corneal transplantation may be combined with cataract surgery to avoid a delayed visual recovery.
Different types of corneal transplant for corneal endothelial failure
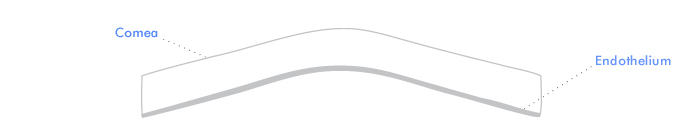
The drawing above is a section through the cornea, which is the clear front part of the eye wall. The corneal endothelium lines the inside of the cornea. Endothelial cells continuously pump fluid out of the cornea. If these cells are not working well, the cornea becomes waterlogged and cloudy. A corneal transplant is then required to replace the endothelium. This transplant can be done in two ways.
Conventional corneal transplantation - PK (Penetrating Keratoplasty)
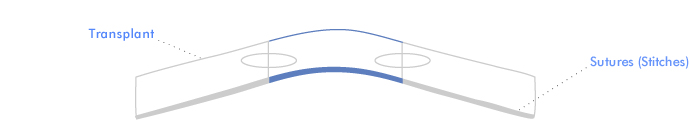
In conventional corneal transplantation, the full thickness of the front of the eye wall is replaced by a disc shaped piece of donor corneal tissue which is sewn into place. The circular wound heals gradually, and the sutures are normally removed one to two years after surgery.
EK (Endothelial Keratoplasty)
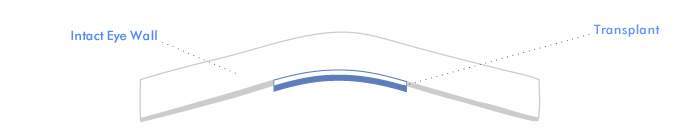
In EK, a new method of corneal transplantation, a healthy new endothelium is transplanted on a thin layer of donor corneal tissue which is floated into place and adheres without sutures. The eye wall is left intact. This helps to preserve a normal corneal shape, normal strength and a normal focussing power for the eye. DMEK is the latest form of EK in which the endothelium is transplanted on its natural supporting layer only (Descemet's Membrane) with no additional tissue.
Outcomes for conventional corneal transplantation
- Around 66% of corneal grafts (two out of three) performed for corneal endothelial failure remain clear for five years or more.
- If the corneal transplant fails (goes cloudy) repeat corneal transplantation is usually possible. But the chances of success diminish with successive grafts. Around 50% of second corneal grafts (one in two) remain clear for five years or more.
- Problems leading to graft failure include: inflammation caused by an immune reaction to the transplant (graft rejection), infection, and raised fluid pressure in the eye (glaucoma). Rejection episodes are more common in repeat corneal grafts.
- With a clear graft, around 75% of patients (three out of four) have improved vision. Vision stays at the same level as before surgery in around 12.5% (one in eight) and is worse in about 12.5%.
- The commonest reason for a disappointing visual result if the graft remains clear is astigmatism (irregular corneal shape giving a blurred focus). Surgery and suture manipulations to correct astigmatism are often required after conventional corneal transplantation.
Endothelial keratoplasty (EK) vs conventional corneal transplantation (PK)
EK, like modern cataract surgery, can be performed through a small self-sealing incision.
Advantages for EK include:
- Greater strength - after EK, an injury to the eye is unlikely to cause eye wall rupture and permanent loss of sight. This means fewer restrictions on activity than after PK.
- Better shape - after EK, changes in the eye wall shape are greatly reduced in comparison with PK. Problems with astigmatism are uncommon, visual recovery is faster, and patients are less dependent on spectacles or contact lenses for good vision.
- No suture problems - two of the commonest reasons for graft failure in PK are rejection and infection. Both problems may be precipitated by suture loosening or breakage. Because there are no sutures on the corneal surface after EK, these problems are avoided.
Disadvantages for EK are:
- An extra optical interface - some light is scattered at the junction between the eye wall and the thin layer of tissue which supports the new endothelial cell layer. This limitation does not apply to DMEK in which no additional supporting tissue is transplanted, and interfacial light scatter for all forms of EK tends to diminish with time.
- Failure to adhere - up to 10% of EK patients (one in ten) require a revision procedure if the graft fails to adhere or at the first operation or fails to clear out subsequently. This is usually performed under local anesthetic. A new air bubble is injected into the eye and the graft is floated back into place.
Combined cataract and corneal graft surgery
Cataract surgery is commonly combined with both PK and EK. This is because cataract surgery can commonly precipitate corneal endothelial failure in patients with Fuch's Dystrophy. In some patients, the need for corneal transplantation is clear. But where doubt exists, cataract surgery is commonly performed first with the proviso that corneal transplantation may be necessary later if the cornea becomes cloudy.
Recovery from surgery
Corneal transplantation can be performed under either general or local anaesthetic. An overnight stay after surgery is often preferred for patients travelling from outside London. The eye is usually sore and watery in the early days after surgery, but comfort quickly improves. Drops are used frequently to help improve comfort, protect from infection, reduce inflammation and promote healing. Patients can usually return to work after two weeks off to concentrate on putting eye drops in hourly or two hourly.
Vision is usually blurred in the early days after a corneal graft. For patients with a conventional graft (PK), three months are required for initial shape stabilisation before a spectacle test is performed to complete the first stage of visual rehabilitation. Vision then usually remains stable until sutures are removed 18 months to two years after surgery. Suture removal produces further corneal shape changes, and further spectacle testing, or revision surgery to correct the corneal shape are often necessary to get the best visual results at this stage.
Visual recovery after EK is usually faster, with the graft clearing rapidly over the first 6 weeks after surgery and relatively early shape stabilisation. Further gains in graft clarity are common in the first six months after surgery.
Corneal transplant rejection
Anti rejection eye drops are usually continued for at least 2 years after EK and PK. It is important to come straight to Moorfields Eye Casualty if, after corneal transplantation, the eye becomes blurred, red or painful at any stage (even many years) after surgery. Most rejection episodes can be reversed, but prompt treatment is necessary to avoid corneal transplant failure. Reduced rejection rates (2% in the first 2 years) are an important advantage for DMEK over other forms of corneal transplantation for corneal endothelial failure all of which transplant more donor tissue than the DMEK technique.
Appointments
For a corneal transplantation assessment with Mr Allan you will need to be eligible for NHS treatment and have a referral from your GP or Ophthalmic Surgeon.
Referrals should be addressed to Mr Bruce Allan, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital, City Rd, London EC1V 2PD
NHS Secretary - Barbara Stacey (email barbarastacey@nhs.net telephone 020 7566 2320)