You are here:
- Procedures / Laser Vision Correction
Laser vision correction
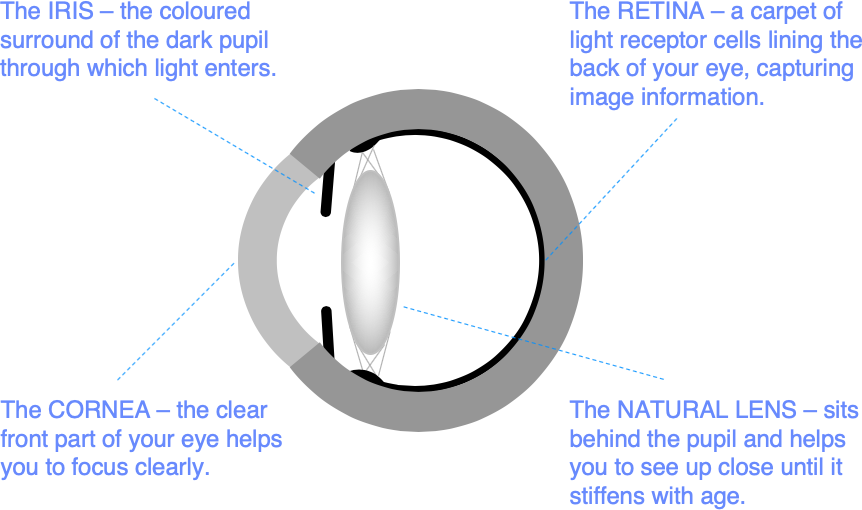
Modern surgical lasers are able to alter the curvature and focusing power of the front surface of the eye (the cornea) very accurately to correct short sight (myopia), long sight (hyperopia), and astigmatism. We can also help correct the need for reading glasses.
Three types of laser vision correction are commonly used: LASIK, TransPRK, and SMILE. Risks and benefits are similar, and all these procedures normally produce very good results in the right patients. Differences between these laser vision correction procedures are explained below.
If you are suitable for laser vision correction, we will discuss which procedure is the best option for you.
What are the benefits?
For most patients, vision after laser correction is similar to vision in contact lenses before surgery, without the potential discomfort and limitations on activity.
Glasses may still be required for some activities after treatment, particularly for reading in older patients.
Over 95% of patients are satisfied with the outcome of surgery, and many describe it as life changing. Although laser vision correction is often bracketed with cosmetic surgery procedures, the benefits are mainly functional. It is designed to make you less dependent on glasses and contact lenses, helping you to lead an active lifestyle more easily.
Short sight and astigmatism normally stabilize in the late teens or early 20s, but natural prescription changes can occur at any stage in life. So, laser vision correction sometimes needs to be repeated.
Who is suitable for laser vision correction?
You must be over 21 years of age and have a stable spectacle prescription. This is normally defined as no change greater than 0.5 units (0.5D) in the last 2 years.
You are most likely to be suitable for laser vision correction if your spectacle prescription is in the range:
- Up to -10.00D of myopia or short sight
- Up to +4.00D of hyperopia or long sight
- Up to ±6.00D of astigmatism
Laser vision correction can be effective for higher prescriptions in the right patients. Conversely, some patients with lower prescriptions may be better suited to lens implantation techniques. We will advise on your best treatment options after reviewing your test measurements and your eye health.
You may not be suitable for laser vision correction if you have other problems with your eyes including cataracts, or problems with eye surface health. We do not normally operate on patients while they are pregnant or breast feeding.
Many contact lens wearers are incorrectly diagnosed as having dry eyes and are told that they are unsuitable for laser vision correction. Eye surface discomfort is common in contact lens wearers and is often treatable. Laser vision correction is often a good solution for patients who are having difficulties with contact lens wear.
What if I am losing my reading vision?
Myopia and astigmatism normally cause poor distance vision from the teenage years on. But hyperopia typically affects people more as they get into their 30s and above. Younger patients with hyperopia often have no problems seeing well. This is because flexibility of the eye’s natural lens allows them to compensate. As the natural lens stiffens with age, hyperopic patients first find themselves more dependent on reading glasses than people with normal sight, and then find that they need glasses for the distance too.
Age related loss of reading vision can often be helped with laser vision correction. From the mid-40s on, we normally aim for good distance vision in one eye, and good vision at arms’ length in the other. With both eyes open, binocular visual input combines to extend the range of focus. Near vision is at least partly restored with relatively little compromise optically. Variations on this approach, marketed under a variety of brand names, have become the default strategy for improving the near range in older patients undergoing laser vision correction.
What are the alternatives?
Lens implantation
Lens implantation techniques that have evolved from modern cataract surgery may be more suitable for some patients.
There are two main categories of vision correction based on lens implantation: refractive lens exchange (RLE) and phakic intraocular lenses (PIOLs).
RLE is identical to modern cataract surgery, but is performed with the main aim of increasing freedom from glasses. RLE is often preferred to laser vision correction for patients in the retirement age group in which the early stages of cataract are common. In RLE, the natural lens is replaced with a lens implant. A variety of different implants are used including multifocal lenses designed to reduce reliance on glasses for near, intermediate and distance vision.
In younger patients, ICL implantation is often a good alternative where the spectacle prescription is outside the normal range for laser vision correction. ICLs are implanted in front of the natural lens without replacing it.
Alternative laser vision correction procedures
The main difference between laser vision correction procedures is speed of recovery. Patients undergoing LASIK are often able to return to work the day after surgery. Visual recovery after SMILE may be slower, and patients undergoing TransPRK may need a week or longer before they are at the driving standard. Although visual recovery can be slower after surface laser treatments or SMILE, patients can return to contact sports sooner, whereas LASIK patients need to wait for a minimum of 1 month. Also, the recovery of eye surface comfort may be slightly faster after SMILE. But differences between techniques are small and mild eye surface discomfort in early period after all forms of laser vision correction is normal. Visual results at 3 months are equally good for all types of laser vision correction.
Continuing in glasses or contact lenses
Laser vision correction is elective. This means you can choose to proceed with it at any time, or not at all. The alternative is staying in glasses or contact lenses.
Glasses are risk free but may limit the range of activities you can do confidently and comfortably – particularly sport and exercise.
Contact lenses provide good all-round vision. They do not mist over during sport and will help you to be more active; but they can be inconvenient when travelling, make water sports more difficult, and should not be worn whilst showering, swimming or during sleep. Contact lens wear is sometimes associated with eye surface discomfort, and may be complicated by sight threatening infection.
Risks and benefits of laser vision correction should be balanced against those for contact lens wear since this is the main alternative for active people considering vision correction surgery.
How do we measure your vision accurately?
We use latest generation wavefront scanners (pyramidal sensors) to enhance the accuracy of your treatment.
Wavefront scanning measures myopia, hypermetropia, and astigmatism directly, with about twice the precision of standard spectacle testing.
Wavefront scanners also measure elements of defocus called higher order aberrations. Higher order aberrations are best understood by thinking of your spectacle prescription as an average of the focusing requirements for light rays entering the eye through different points on the eye surface.
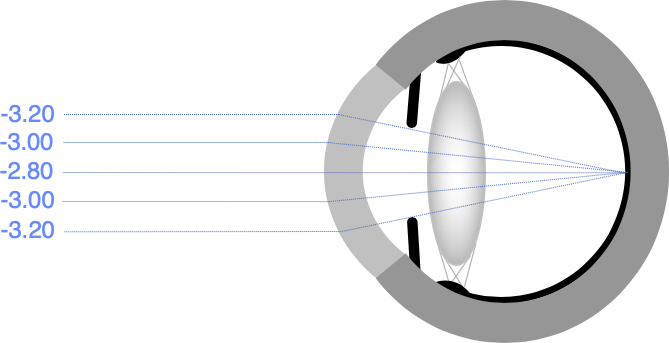
If your spectacle prescription is, for example, -3.00D, this may be an average of -2.80D for rays entering through the centre of the cornea and -3.20D for rays entering around the edge.
Current wavefront-guided laser treatments do not routinely produce better vision than spectacles and contact lenses, but they can help to improve overall visual quality and treatment accuracy in the right patients. We will discuss your suitability for wavefront-guided treatment with you at your preliminary consultation.
How is laser vision correction performed?
All laser vision correction procedures are performed using eye-drop anaesthetic. A spring clip gently holding your eyelids apart allows you to blink safely during surgery. You will be lying down throughout. It is usual to operate on both eyes, and the surgery typically takes about half an hour. You can return home on the same day as surgery.
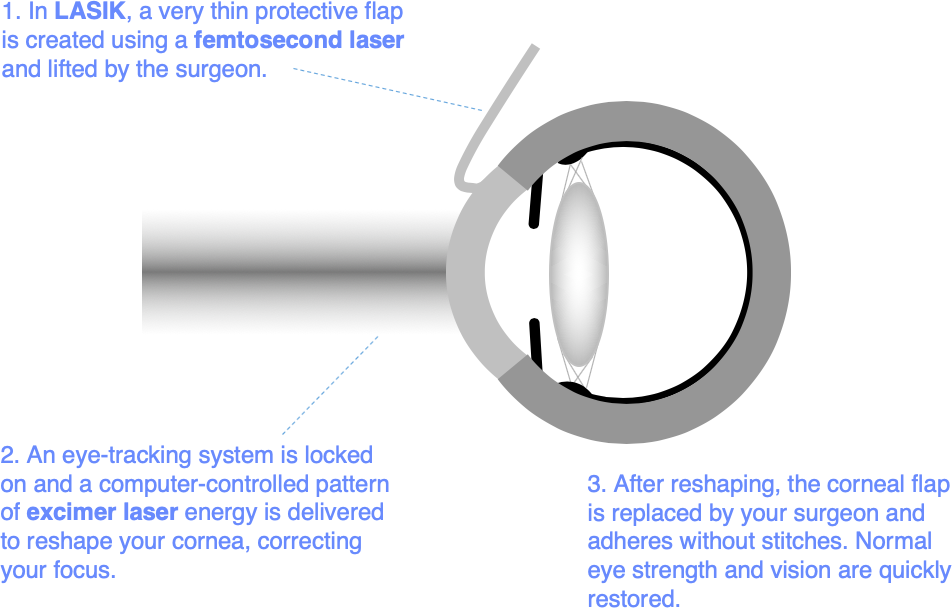
LASIK
LASIK (laser in situ keratomileusis) is performed using 2 lasers: one (femtosecond laser) to prepare a thin protective layer (the LASIK flap), which is lifted up before a second (excimer laser) removes a lens shaped piece of tissue to reshape the cornea beneath. The protective layer is then smoothed back and sticks in place and without stitches.
TransPRK
Surface laser treatments (PRK, LASEK, and most recently transepithelial photorefractive keratectomy – TransPRK) use the same excimer lasers used in LASIK to perform an identical removal of a lens shaped piece of tissue immediately beneath the clear skin layer of the cornea. The clear skin layer regrows over a period of about a week, then smooths off optically to complete the visual recovery over the next three months.
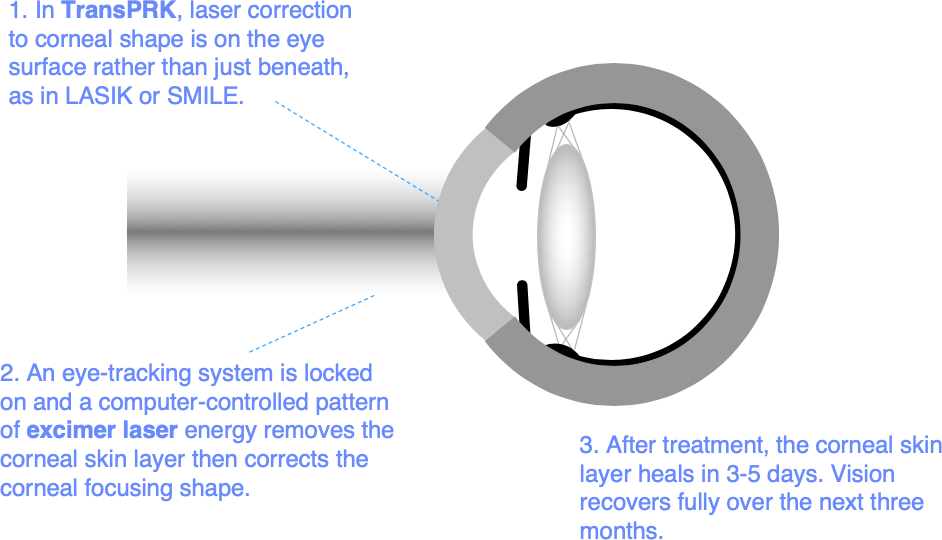
Surface laser treatments are the safest option for some patients. But while the skin layer is re-growing after treatment, the eye surface is normally very sore. This is one of the main differences between surface laser treatments and LASIK or SMILE, which both aim to keep the corneal skin layer intact.
All surface laser treatments produce similar results, and the only difference between them is the way in which the corneal skin layer (the corneal “epithelium”) is removed. In PRK and LASEK the skin layer is removed by the surgeon - in LASEK dilute alcohol is applied to loosen the skin layer first. The Schwind Amaris 1050RS excimer laser system we use at Moorfields is able to remove the skin layer as part of the reshaping treatment. This is called TransPRK. The area of skin layer removal in TransPRK is reduced to the minimum required for reshaping the cornea beneath, shortening recovery time by 1 to 2 days in comparison with PRK and LASEK.
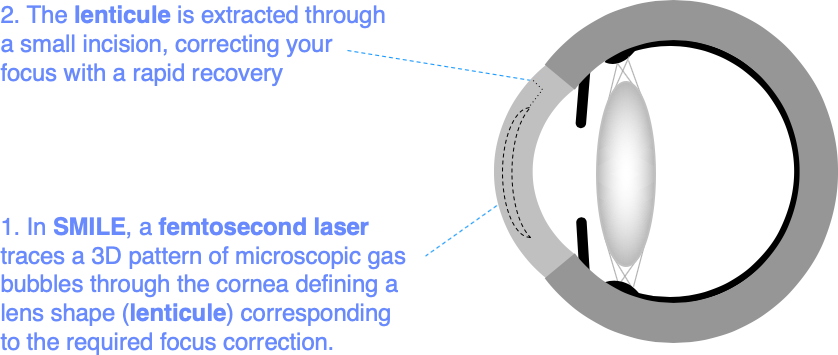
SMILE
SMILE (Small Incision Lenticule Extraction) uses a femtosecond laser of the same type used to create a LASIK flap to define a lens shaped piece of tissue that is removed by the surgeon through a small incision to correct focus. This is like LASIK without the LASIK flap, but the thickness of tissue removal is slightly greater and the tissue may be removed from slightly deeper in the cornea. End results are similar to those for LASIK and surface laser treatments.
Which laser systems do you use at Moorfields?
Because Moorfields Eye Hospital is a flagship location for manufacturers of laser equipment, we are able to select from all the leading laser platforms and renew our equipment regularly. We are currently using the Schwind Amaris 1050RS excimer laser platform, which combines a proven clinical track record with the best options for wavefront-guided LASIK, TransPRK, and specialised laser treatments to correct problems with visual quality in conditions such as keratoconus. We also use the Zeiss Visumax 800 femtosecond laser. Advantages for this femtosecond laser are a better fit to the contours of the eye for more comfortable treatment, better automated guidance for treatment precision, and industry leading SMILE capabilities.
What are the risks?
In all forms of eye surgery, problems can occur during the operation or afterwards in the healing period. Problems can result in permanent, serious loss of vision (vision worse than the driving standard in the affected eye that cannot be corrected with glasses or contact lenses). More commonly, problems can be corrected with changes in medication or additional surgery. Typically, these additional operations feel like the original surgery and have a similar recovery period.
Loss of vision
Permanent, serious loss of vision is rare after laser vision correction. In the worst likely scenario, a form of corneal transplantation may be required to replace a damaged block of tissue in the cornea. Problems that can lead to the need for transplantation include scarring after infection or an abnormal healing response, and an unstable corneal shape – also called corneal ectasia. These problems occur infrequently, and can often be corrected without transplant surgery. Less than 1 in 5000 patients require a corneal transplant to restore vision after laser surgery, and good vision can normally be restored when transplantation is necessary although glasses or contact lenses may be required.
Additional surgery
Much more commonly, a second operation is needed to correct a problem occurring at the time of surgery or afterwards. This would normally be a procedure that feels similar to the original laser vision correction, with a similar recovery period. Some of these procedures need to be repeated. If you have a problem, we will explain what it is and why further surgery is required. Up to 1 in 10 patients require some form of additional surgery in order to get the best result.
Risks of contact lens wear
Continuing in contact lenses is often the main alternative for people considering sight correction surgery. If you follow the right safety advice, contact lens wear is low risk; but approximately 1 in 3000 wearers each year will develop a serious corneal infection.
To minimise this risk, you should not swim or shower in contact lenses, and should not wash them in tap water. Sleeping in contact lenses, including those designed for overnight wear, increases the risk of infection significantly. Soft, daily disposable lenses are safer than non-disposable lenses.
What are the side effects?
Side effects are problems which most patients experience to some degree after surgery. They normally improve with time, but do not always resolve completely.
Vision
Most patients experience some light scatter side effects in the early period after laser vision correction, particularly those who have treatment for higher spectacle prescriptions. These can take a variety of forms including glare, halos, floaters, starbursts and ghost images. Increased flare from oncoming car headlights is a common symptom, and night driving may be difficult at first. With modern laser systems, visual side effects are usually mild and improve within a few months. Lasting problems are unusual, but may still occur.
Eye comfort
Other common side effects are intermittent blurring (variable vision) and eye surface discomfort (dry eye symptoms). Both are caused by reduced stability of the tear film between blinks. Tear film stability improves over a few months after treatment as the corneal surface heals. During the healing period, most patients are able to stay comfortable using tear supplements when required. Eye comfort usually returns to normal within a few months of treatment and, for contact lens wearers in particular, may be better after laser vision correction than before. For patients with a normal eye surface prior to surgery, lasting problems are unusual.
Eye Appearance
Red blotches are often visible on the white of the eye after any form of eye surgery, and are particularly common after LASIK. These are called subconjunctival haemorrhages, and are caused by a small leak of blood under the clear membrane (the conjunctiva) covering the white part of the eye wall. Although they can be quite unsightly, red blotches are temporary, and do not affect eye health; but they can take up to 6 weeks to go away completely.
Will laser vision correction affect my future eye health care?
If you develop a new eye health problem in later life, laser vision correction should not prevent you having successful treatment. Common eye health problems like diabetic retinopathy and age-related macular degeneration are monitored and treated as normal after laser vision correction.
Laser vision correction can affect eye pressure measurements used to check for glaucoma, causing them to under-read, especially in patients who have had treatment for high myopia. Corrections to eye pressure measurement can be applied to help ensure that glaucoma is picked up at an early stage and treated effectively; but it is worth reminding your optometrist or doctor that you have had laser vision correction when they are checking for, or treating glaucoma. A record of your last spectacle prescription before laser vision correction may help them to calibrate your eye pressure readings more accurately.
Laser vision correction can reduce the accuracy of focus correction after future cataract surgery. Any detrimental effect is small, and is reducing as more patients who have had previous laser vision correction are entering the cataract age group and modifications to lens implant selection calculations are becoming better understood.
How can I reduce the risk of problems?
You can eat and drink normally before surgery, and should take any regular medication as usual.
You have to be awake for laser vision correction so that you can look up to a target light. This helps you keep your eye in the right position during treatment. Stay as relaxed as you can during the surgery, and try to keep your head still after we have positioned it comfortably for you. Most people are anxious prior to surgery. We are used to this, and will talk you through the procedure, encouraging you at every stage. Keep your breathing calm and tell us if you need a break. An anti-anxiety, muscle-relaxing drug such as diazepam can be helpful, particularly if you tend to squeeze your eyes shut when they are being touched. Let us know if you are worried, and we will help you to relax.
Modern laser systems either hold the eye still with gentle suction or have accurate tracking systems that follow eye movements during surgery, and a spring clip is used to hold the eyelids apart. So, you should not worry too much about moving or blinking during the procedure. But try to listen to instructions and keep your eyes on the fixation light when asked to do so.
It is important to keep the eyes well lubricated in the first few hours after treatment, particularly after LASIK. Stay awake, but rest with your eyes closed when you can, and use the lubricant drops you will be given frequently.
You can wash and shower normally from day one after LASIK or SMILE, and once the bandage contact lenses used after TransPRK have been removed – typically on day 4 to day 7 after surgery. We recommend no swimming for a week and, after LASIK, no contact sports for a month. Non-contact sports such as gym and jogging can be resumed from day one after surgery.
Set a smart phone reminder and use the antibiotic and anti-inflammatory drops as prescribed to help the eyes to heal well. It is good to leave at least 2 minutes between different types of eye drop so that they each absorb well before the next drop is applied. If you miss the first time or you are not sure, applying a second eye drop is no problem.
Some variability of vision and comfort is normal in the early weeks after surgery, and patience is required. But you should not be afraid to contact us if you have any concerns, or if you have an injury to the eye. You should contact us without delay if you have increasing pain, light sensitivity, redness, blur or an injury to the eye followed by pain, blur or watering. You will be given Mr Allan’s mobile phone number for emergency contact after surgery. The practice management and the laser nursing team are also available for informal advice. The Eye Casualty Department at Moorfields Eye Hospital is open for emergency review 24 hours a day, 7 days a week.
You may not be aware of a problem that requires treatment in the healing phase. So, make sure you attend your review appointments even if your eyes feel good.
Appointments and Enquiries
If you wish to arrange a preliminary consultation, please telephone Angelique Thomas on 020 7566 2156 or 07484 081815 (or from outside the UK +44 20 7566 2156 or +44 7484 081815) or email moorfields.ballan@nhs.net
Additional information
This information is adapted from Standardised Patient Information on Laser Vision Correction published by the Royal College of Ophthalmologists. This information can be downloaded here.
