You are here:
- Procedures / YAG Capsulotomy
YAG laser capsulotomy
In cataract surgery, an intraocular lens (IOL) is implanted within your natural lens capsule. The lens capsule is a thin clear membrane, a bit like the skin of a grape, which encases the natural lens.
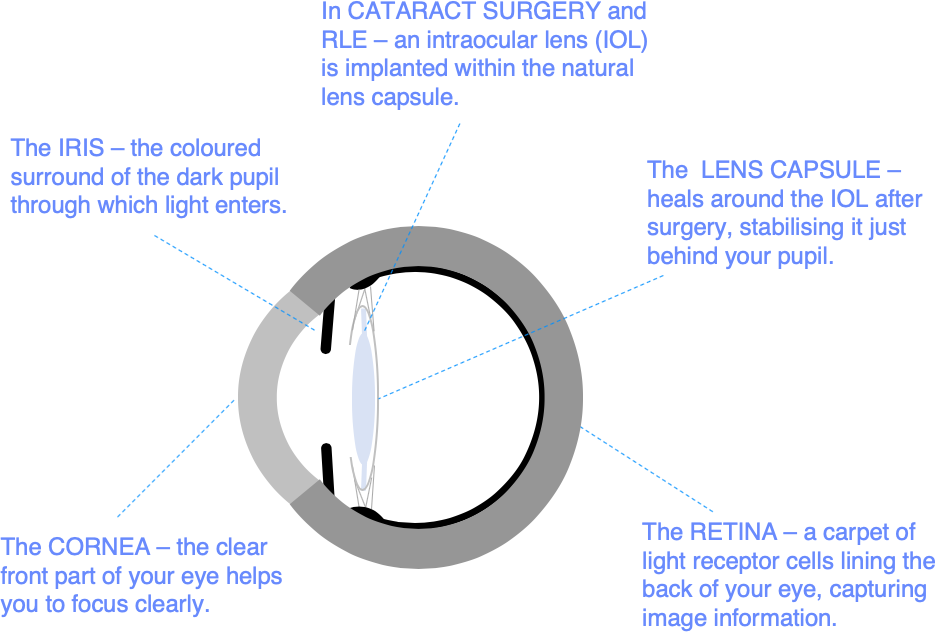
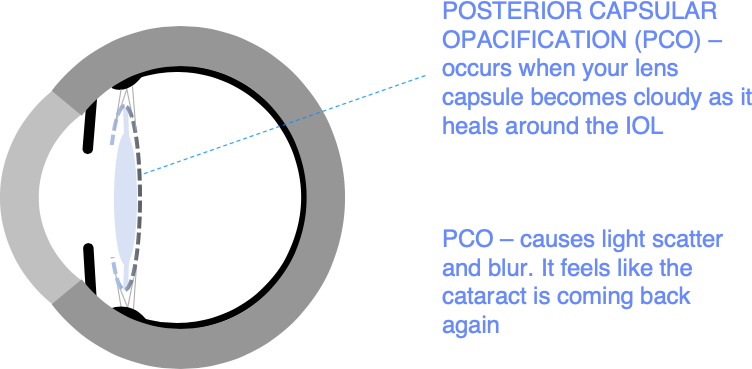
In the months after surgery, your lens capsule shrink-wraps the IOL and stabilises it definitively in the natural position just behind your pupil. Sometimes your lens capsule becomes opacified during this normal healing process, your visual quality gradually deteriorates, and it can feel as if the cataract is coming back.
This common problem after cataract surgery or refractive lens exchange (RLE) is called posterior capsular opacification (PCO). PCO affects up to 1 patient in 5 after cataract surgery. It typically becomes noticeable 1-3 years after surgery, but it can be present at the time of surgery in some types of cataract (posterior subcapsular cataracts) and it can also occur many years later.
PCO is corrected by cutting through the thin, frosted lens capsule to restore a clear pathway for light to focus on the retina. This is done with a specialised (YAG) laser in a painless 15-minute corrective procedure called YAG laser capsulotomy. This normally restores vision to the level it was originally at after cataract surgery.
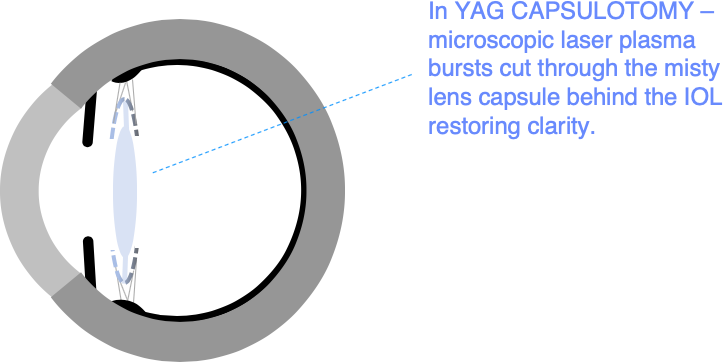
YAG lasers are in a class of lasers called ‘photodisruptors’. They work by focusing a very brief pulse of laser light at a precise point in 3D space. Concentrating light energy in this way creates a tiny ‘explosion’ of plasma that cuts through your lens capsule. Light is transmitted harmlessly through the eye before and after this microscopic focus point.
How is YAG capsulotomy performed?
YAG capsulotomy We start by dilating your pupils. You are sitting up for treatment, and eye drops are used to numb the eye. A contact lens is then held against your eye to help keep the eyelids out of the way, steady your eye, and focus the laser.
You look straight ahead at a fixation light with your other eye. The procedure is not painful, and the laser light is not visible, but you can sometimes see the red laser aiming beam, and you may be aware of a clicking sensation in the eye caused by the microscopic laser pulses.
There are no limitations on activity after treatment. You may be a bit light sensitive initially, but discomfort is normally minimal. We give you drops to put in for a few days after treatment to minimise any inflammation inside the eye.
What are the benefits?
YAG capsulotomy should restore your vision to the level it was at in the early months after your cataract surgery, before PCO became a problem.
Vision normally improves somewhat within 24 hours of treatment, with gradual further improvement over the next few months as your lens capsule contracts to clear the pathway of light through your pupil fully.
What are the risks?
Risks associated with YAG laser capsulotomy are well contained. Briefly, these are: IOL damage (approximately 1 in 100 patients) - correctable with an operation similar to cataract surgery in which the damaged IOL is exchanged for a new one; cystoid macular oedema (approximately 1 in 100 patients) - a mild waterlogging or bruising response in the retina which causes a temporary reduction of vision lasting, typically, 6 to 9 months; and retinal detachment (approximately 1 in 350 patients).
Some floaters (appearing like moving flies/cobwebs in the field of vision) in association with capsular debris displaced into the (vitreous) gel behind the lens are normal after YAG capsulotomy. But a sudden new shower of floating opacities, lightning flashes, or a curtain like loss of the visual field are danger signs that a retinal detachment may be in progress.
If you experience sudden visual loss after either cataract surgery or YAG capsulotomy, you should always go straight to a Casualty Department for an emergency eye examination. 9 out of 10 retinal detachments are repaired successfully at the first attempt, but the chances of success are enhanced by treatment at an early stage.
Appointments and enquiries
To arrange a private consultation, please telephone Angelique Thomas on 020 7566 2156 or 07484 081815 (or from outside the UK +44 20 7566 2156 or +44 7484 081815) or email moorfields.ballan@nhs.net
For NHS treatment with Mr Allan’s team at Moorfields, you will need a referral from your GP or Ophthalmic Surgeon. Referrals should be addressed to Mr Bruce Allan, Consultant Ophthalmic Surgeon, Moorfields Eye Hospital, City Rd, London EC1V 2PD. If you have any difficulty with your NHS referral, please call Barbara Stacey, NHS secretary to Mr Allan on 020 7566 2320, or email barbarastacey@nhs.net.
